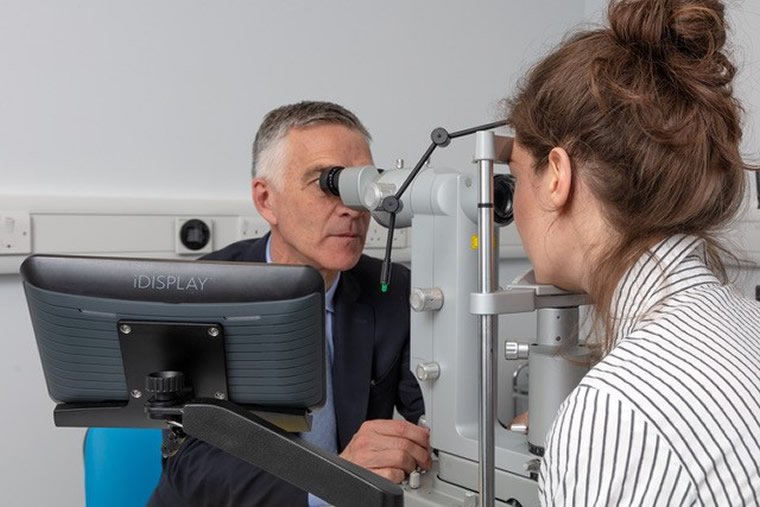
Professor Williamson is considered an international authority in Vitreoretinal Surgery and often receives referrals for secondary opinions from colleagues, both nationally and internationally. He also has extensive experience in undertaking most types of general ophthalmic procedures, including modern techniques in cataract (phacoemulsification) surgery.
Read about the conditions which Professor Williamson manages together with some general information about the treatment options available to patients. For any questions or to request a private consultation please refer to the Contact page of this website.
Retinal Detachment
The retina is the lining of the back of the eye, which allows the eye to see. If a hole appears in the retina it will detach rather like wallpaper peeling off a wall. The retina cannot work when it is detached. The only way to repair the retina is by operation to find the hole or holes and sealing them.
Certain symptoms may indicate retinal disease, these include loss of vision, visual distortion, flashes and floaters, a shadow in the vision, blurred vision and / or patchy vision. Patients experiencing these symptoms should seek advice from an opthlamologist.
Treatment
The retina can be repaired in one of two ways:
- The hole can be sealed by sewing a small piece of plastic onto the outside of the eye, creating a dent in the eye ball, which will close the hole. You may be able to feel the plastic on the eye after the operation.
- Alternatively, it is possible to go inside the eye and, by removing the jelly in the eye (known as the vitreous), a gas bubble can be inserted to support the retina. This procedure is known as a vitrectomy and is performed by making three small incisions in the eye. The operation takes approximately one hour to perform. The gas bubble will float inside the eye and close the hole. Laser or freezing treatment is used to seal the hole.
The surgeon will decide which type of surgery is most appropriate for each individual patient. The eye does not need the vitreous jelly – it will fill the space with a watery fluid.
Posterior Vitreous Detachment (PVD)
Posterior vitreous detachment (PVD) is the most important event in retinal surgery. It causes many of the conditions seen by a retinal surgeon. It is very common over the age of 40 years and more often in myopes. PVD may cause symptoms of floaters and flashes in the eye. If you suffer a sudden onset of these symptoms you should seek examination of your eyes by a retinal specialist. In 10% of patients with acute PVD a retinal tear can be found and will need treatment with laser. Untreated retinal tears can lead to retinal detachment which can severely reduce your vision.
Macular Degeneration
What is macular degeneration?
This is an aging change in the eye which damages the macula of the retina thereby reducing central vision. Unfortunately, macular degeneration is common in the elderly and can cause irreversible central visual loss. Peripheral vision is maintained even when the patient has lost reading vision.
There are two main types:
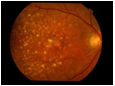 Dry: Most patients with macular degeneration suffer from the dry form of the degeneration producing a gradual weakening of the retina. This can be seen as yellow deposits in the retina called Drusen or as areas of increased or decreased pigmentation of the retina. It is important to have the eye examined as for some types of dry degeneration (for example the eye on the right) special vitamin and antioxidant tablets have been found to reduce the risk of progression to visual loss.
Dry: Most patients with macular degeneration suffer from the dry form of the degeneration producing a gradual weakening of the retina. This can be seen as yellow deposits in the retina called Drusen or as areas of increased or decreased pigmentation of the retina. It is important to have the eye examined as for some types of dry degeneration (for example the eye on the right) special vitamin and antioxidant tablets have been found to reduce the risk of progression to visual loss.
It is useful to seek advice on the severity of your macular degeneration as the risk of progression to visual loss varies from 3% to 40% over 5 years depending on the appearance of the retina.
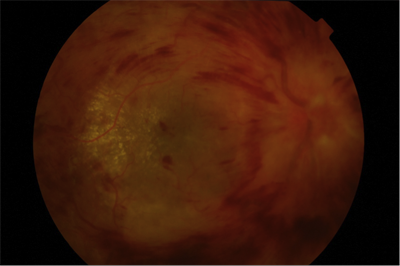
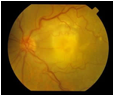 Wet: A few patients will produce a more severe form where a blood vessel membrane appears in the eye as shown on the left. This causes damage to the retina with severe loss of vision often in both eyes. In the early stages the vision distorts followed later by loss of central vision.
Wet: A few patients will produce a more severe form where a blood vessel membrane appears in the eye as shown on the left. This causes damage to the retina with severe loss of vision often in both eyes. In the early stages the vision distorts followed later by loss of central vision.
Anti VEGF Injections
Anti VEGF drugs, namely Ranibizumab (Lucentis) and Aflibercept (Eylea), restrict the growth of blood vessel membranes in wet ARMD. These block the action of a hormone in the retina called VEGF which makes blood vessels grow. The drugs are injected into the eye under local anaesthesia and have been extremely useful for maintaining or improving vision in this otherwise blinding condition.
The use of these drugs may involve monthly injections and repeat injections over years.
Macular Surgery
What is the Macula?
The macula is the part of the retina which is needed for fine detail such as reading or recognising faces. It contains delicate receptors called cones which also provide colour vision. Distortion of vision (straight lines appearing to look bent, check your eyes by observing a rectangular window frame one eye at a time) is a common symptom of macular disease.
Macular Hole
A hole can appear in the macula. This has a tendency to distort and reduce the vision. It is possible to close the hole to improve the vision by vitrectomy operation. This involves removing the jelly of the eye (vitrectomy) and inserting a gas bubble which remains in the eye for a few weeks. The gas bubble floats in the eye and pushes on the hole.
Please note that extreme posturing regimes (e.g. face down) can be avoided with modern macular hole surgery, and is rarely used by Professor Williamson.
- There is a chance the eye will develop a cataract in the next few years.
- The patient must not travel by plane whilst the gas bubble is in the eye.
- 2-6 months may be required for the eye to recover its best vision after surgery.
Macular Pucker
Sometimes a membrane appears that wrinkles the retina – this is known by different names including cellophane maculopathy, epiretinal membrane and macular pucker. A macular pucker blurs your vision and causes distortion (bending or twisting of straight lines). It is possible to operate to try to remove the membrane. The operation involves removing the jelly of the eye (by way of a vitrectomy) and surgically peeling the membrane off the retina. This operation is usually effective in reducing the distortion and improving the vision. A cataract often appears afterwards.
Anti VEGF Injections
Anti VEGF injections are currently being used to reverse swelling in the retina (known as cystoid macular oedema) which arises as a result of a variety of conditions including diabetes and retinal vein occlusion.
Surgery for Diabetic Patients
Diabetic retinopathy is a condition whereby damage occurs to the small blood vessels in the retina of the eye. This may cause swelling in the retina, ischaemia (low oxygen) in the retina and more severe complications, which can lead to blindness.
The mainstays of treatments are laser therapy to the retina or injections of Anti-VEGF drugs into the eye. In some patients with diabetes more extensive surgery is required – there are two main reasons why a patient with diabetes may need surgery:
- Diabetic Haemorrhage; and / or
- Diabetic Retinal detachment
Diabetic Haemorrhage
Diabetes causes abnormal blood vessels to appear in the eye. Laser treatment is used to try to prevent these occurring. These blood vessels are fragile and bleed easily. Sometimes they bleed into the jelly of the eye (the vitreous) reducing vision. Where this has occurred, the vitreous and the bleed are removed by way of an operation known as a vitrectomy and more laser is subsequently applied.
Diabetic Retinal Detachment
Abnormal blood vessels produce scarring which in turn can produce a retinal detachment. To treat this the vitreous is removed and the scars are dissected off the retina. A bubble of gas may be used to support the retina.
When operating on an eye with diabetic retinal detachment, there is a chance a cataract will develop within the next few years.
Post operatively, these patients are prohibited from travelling by plane whilst a gas bubble is in the eye. Your surgeon will advise you when it is safe for you to fly again.
Uveitis and Inflammation
The eye may suffer inflammation or infection requiring intervention by the vitreoretinal surgeon.
What is inflammation?
Sometimes the body may produce a reaction against itself. This happens commonly in the joints or skin and also in the eye. This produces a condition called uveitis.
Uveitis usually only affects the front of the eye and can be treated by drops. Sometimes uveitis affects the back of the eye including the retina and vitreous. When this happens the retina can be damaged and the vitreous become opaque with proteins and cells. These may require vitrectomy surgery to repair.
What kind of infections affect the retina?
Almost all kinds of organism can infect the back of the eye:
- Bacteria after trauma or surgery
- Viruses giving retinal blood vessel inflammation
- Fungi such as candida
- Others such as toxoplasma and toxocara
The retinal surgeon may be required to insert antibiotics or to remove the infection by vitrectomy.
Cataract Surgery
What is a Cataract?
A cataract is formed when the lens of the eye has become opaque, thereby reducing or blurring the vision. Car headlights or bright sunshine may cause problems in patients with cataracts because the cataract scatters light and causes glare. Cataracts are generally seen in patients over 60 years of age however, younger patients may also be affected. Most people over the age of 70 have some signs of cataract.
Eventually, if left untreated, the cataract will affect almost all of the vision however, most patients opt for surgery before this stage in order to restore their vision. Thankfully, advances in modern cataract surgery (which is often also referred to as phacoemulsification surgery) means that the success rates are very high. Cataract extraction and prosthetic lens implantation is the most common surgical procedure on the eye.
Modern Cataract Microsurgery
During surgery the cataract, and therefore the natural lens of the eye, is extracted. To allow the eye to focus, a prosthetic lens implant is inserted. Measurements (known as biometry) are taken prior to the surgery in order to ensure that the correct lens implant is used. This usually allows the surgeon to aim for a particular focus for the eye post-operatively.
In addition, there are premium prosthetic lenses available such as toric lenses and multifocal lenses which can be inserted, the former aim to reduce astigmatism and the latter aim to correct for both near and far vision simultaneously. These options can be discussed during your initial outpatient appointment.
A cataract operation is usually performed under local anaesthetic as a day case and takes approximately 15-20 minutes to complete.
Most patients notice that their vision is significantly improved following the surgery.
View or download full information in PDF format
View or download our Cataract After Care Booklet
Trauma
Unfortunately the eye is prone to injury this can be separated into minor or severe trauma.
Minor Trauma
Corneal Abrasion
A scratch on the surface of the eye may cause a loss of the outer surface of the cornea called an abrasion. This is painful but can be easily treated and tends to heal very quickly within 24 hours. Common causes of injury are scratches / abrasions from fingernails, twigs or contact lenses.
Foreign Body
Specks of dust may become stuck under the eyelids causing irritation when blinking. Fragments from some power tools such as grinders may become lodged in the cornea. These need to be removed and antibiotic drops given to avoid infection in the eye. Sometimes foreign bodies in the cornea leave rust behind that needs to be cleaned off. Other foreign bodies can enter the eye and these must be thoroughly investigated and treated.
Severe Trauma
The eye is delicate and does not cope with injury well. There are four main types of severe trauma to the eye
Intraocular Foreign Body
Something has entered the eye (e.g. a tiny piece of metal from someone hammering and chiselling or from fireworks or air gun pellets). These can cause damage to the internal structures of the eye and infection.
Wearing protective goggles during any sort of activity using power tools, metal tools involving hammering, strimmers, rotating blades is absolutely essential to avoid this complication.
Penetrating Injury
Sharp objects can injury the eye and lacerate the outer surface of the eye. Often these occur in assault, road traffic accidents or childhood accidents. Surgery will be required to try to repair the eye.
Contusion Injury
Sometimes the eye is hit by an object but the eye stays intact. Unfortunately, there may still be a severe degree of injury. This is commonly caused by assault of an individual but is also seen in a variety of sports. Squash and badminton are particularly likely to result in injury because of the close proximity of the players. The wearing of protective goggles is advised.
Scleral Rupture
Sometimes the eye is hit by an object but the eye stays intact and the outer layer of the eye is bursts. This is a severe injury and will need surgery to try to redeem the situation.
General Eye Conditions
Chalazion and Stye
A chalazion is a cyst on the eyelid caused by a build up of secretions in the glands. A cyst is a round and usually painless swelling on the eyelid. Most often these will only shrink over many months and it is best to go forward to a small surgical procedure to drain the cyst. This can be performed under local anaesthetic and takes a few minutes.
A stye is a painful swelling of the eyelids caused by infection of the glands of the lid. It is usually treated by antibiotic ointment and hot spoon bathing.
Blepharitis
The eyelids contain numerous glands some of which provide a fatty layer on the surface of the tear film. These glands can become inflamed of infected. In addition to lid hygiene sometimes antibiotic tablets are helpful to improve the lids and the skin condition.
Hot Spoon Bathing
Heat a wooden spoon in warm water. Remove the spoon and wrap it in cotton wool. Make sure the spoon is warm but not too hot to cause injury and place it on the stye for a few minutes at a time. This helps to allow the stye to discharge and then go away.
To prevent recurrence lid hygiene can be used.
Lid Hygiene
In order to help the glands of the eyelids secrete and therefore avoid blepharitis or the formation of styes or chalazia, massage of the eyelids is useful.
Use a cotton bud on the outside of the eyelids and massage uowards for the lower lids and downwards for the upper lids.
In addition flaky deposits on the edge of the eyelids can be removed by the use of dilute baby shampoo on the cotton bud.
Use antidandruff shampoo when washing your hair as this may also help.
Other Treatments
- Flaxseed oil supplements
- Lipiflow therapy
- Meiboflow therapy
- Systemic antibiotic therapy
Conjuctivitis
This is inflammation of the eye leading to a red eye with watering, stickiness or discharge. This can usually be treated with drops once an ophthalmologist has determined the type of conjunctivitis. If you have an infection of the conjunctiva please avoid sharing towels with other individuals and wash your hand to try to prevent the spread of infection.
Dry Eye
As we age the tears may become less effective and artificial tears may need to be used to keep the eye moist. Dry eyes cause irritation and rare severe forms can damage the surface of the eye.
Retinal Vein Occlusion
What is retinal vein occlusion?
Retinal vein occlusion is caused by a blockage of the blood vessels in the eye, the retinal veins. These blood vessels drain the blood out of the retina. It is like a water pipe being blocked in your house. This causes pressure to build up in the system and leaks to appear. The retina cannot work well when it is swollen which causes a reduction in your central vision often making the vision patchy.
Bleeding and swelling in a patient with retinal vein occlusion
Are there any treatments?
Steroids, AntiVEGF injections and laser to the retina can be used to restore or stabilise vision in retinal vein occlusions in some patients. They have possible complications, which you need to discuss with your surgeon.
What will happen to the eye?
Many patients with this condition will have permanently reduced vision afterwards. The whole process takes 12 months to settle down during which time your ophthalmologist will need to monitor the eye for complications every 1-2 months. If the blockage is severe or becomes severe you may need treatments such as laser or surgery.
Do I need any investigations?
There are a number of investigations, which you may have including blood tests and photographs.
The following simple steps should be taken.
You should drink plenty of water and avoid dehydration
The following activities should be avoided or restricted:
- Long journeys by air
- Heavy exercise
- Heavy drinking of alcohol
- Going to high altitude
Anatomy of the Eye
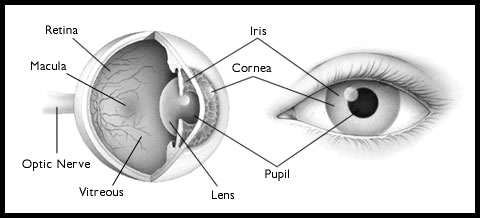 The eye is like a biological digital camera with a lens apparatus at the front (the cornea and lens) and an image processing unit at the back (the retina) which sends images to the brain via the electrical wiring (the optic nerve). The pupil and iris act as the lens aperture. The most common problem to affect the lens apparatus is cataract (clouding of the lens). Many problems can inflict the image processor (retina) including retinal detachment. The eye is spherical in shape and therefore must have a pressure greater than atmospheric pressure to stay ‘inflated’. Uncontrolled pressure can cause glaucoma. In the middle of the sphere is a cavity filled with a clear jelly (the vitreous). Ageing of the vitreous causes many of the problems encountered in the retina including macular holes and pucker.
The eye is like a biological digital camera with a lens apparatus at the front (the cornea and lens) and an image processing unit at the back (the retina) which sends images to the brain via the electrical wiring (the optic nerve). The pupil and iris act as the lens aperture. The most common problem to affect the lens apparatus is cataract (clouding of the lens). Many problems can inflict the image processor (retina) including retinal detachment. The eye is spherical in shape and therefore must have a pressure greater than atmospheric pressure to stay ‘inflated’. Uncontrolled pressure can cause glaucoma. In the middle of the sphere is a cavity filled with a clear jelly (the vitreous). Ageing of the vitreous causes many of the problems encountered in the retina including macular holes and pucker.
Investigations
What investigations might be performed?
The complexity of retinal disorders means that sometimes extra investigations will be needed to allow diagnosis of your condition and to allow a plan of action to be made. Many of these investigations involve state of the art technology, most are entirely non invasive and provide wonderful insights into the working of your eye.
Here are some of the common investigations used:
Optical Coherence Tomography
This uses low dose laser light to scan the macula of the eye producing images of slices of the retina. It is particularly useful for identifying macular problems.
Ophthalmoscopy
The surgeon will use a number of special optical tools which allow a magnified 3D image to be obtained of the various parts of the eye. Using high powered lenses the retina can be thoroughly examined.
Photography, Fluorescein Angiography and ICG Angiography
Using special cameras it is possible to photograph the retina to monitor disease. Using special dyes (fluorescein and indocyanine green, ICG) it is possible to look for damaged areas of the retina or choroid (the blood vessels behind the eye). This is especially important when looking for the membranes which destroy vision in macular degeneration as shown on the left.
Ultrasound
This uses sound waves to build up a picture of the eye and is especially useful when there is no view of the eye by ophthalmoscopy, e.g., in vitreous haemorrhage. The cause of the haemorrhage can be looked for:
- Diabetic retinopathy
- Retinal tear or detachment.
- Retinal vessel occlusion
- Macular degeneration
Doppler signals can be obtained to allow identification of individual blood vessels in the eye.